flyingcheesehead
Touchdown! Greaser!
As MAKG said, in fact the air you breathe is changing temperature pretty instantly, and except for really extreme situations, the wet warmth of your nose, mouth, airways, lungs overwhelms the relatively low specific heat of the air entering your lungs.
Now we're starting to make more sense!
During normal nose breathing, air is heated to about 97F and has an 80-90% relative humidity by the time it reaches the carina (that bit where your trachea splits into bronchi to go to your lungs separately). Things go a bit slower than that if you're breathing through your mouth,
Speaking from an engineering mindset, though, when the air reaches the carina there would be a temperature distribution - It'd be 97-98 degrees near the edge of the trachea, but the air in the middle, which hasn't yet had direct contact with warm, most tissues, should still be closer to its original temperature.
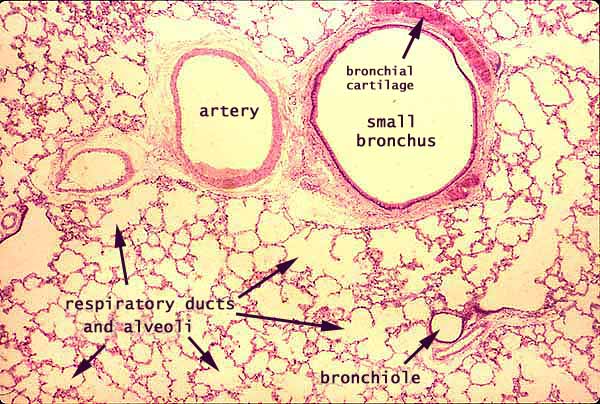
but by the time air gets to the alveoli (the air sacs in your lungs that actually do gas exchange with blood), it's safe to assume in all but the weirdest situations (antarctic explorers or mountain climbers caught out) that the air is body-temperature and fully saturated.
How big are alveoli? How big are the tubes by the time they get there?
Exercise is definitely more difficult in heat and humidity. That's because your body relies on the fact that it's dumping heat and water into the air you're breathing in order to cool down. (We may not be dogs, but we still use panting for cooling to some degree.) If the air coming in is already hot and humid, the body isn't pumping that heat and evaporative air into the air for exhalation, and so there is more heat strain on the body overall. Part of the response (though a smallish part) is to try to breathe more (and therefore feel like you can't get enough air) in order to get that cooling going.
A bigger part of the response is that (unlike dogs) we do most of our physiologic cooling through our skin: by sweating and dilating the capillaries in our skin. (If we make our skin warm, that heat is lost by conduction, convection, radiation, and sweat evaporation.) The dilation of capillaries all over the skin drops the resistance to bloodflow in the overall body system, and means your heart needs to pump all the harder to maintain pressure on the system.*
This effect -- and the resultant workload on the heart -- is higher in hot and humid environments as conductive/convective heat loss is less (heat) and evaporative loss from sweat is less effective (humidity). That cardiac load feels very much like air hunger and "can't quite catch my breath" and "can't go any harder, but it's not because of my legs".
Great explanations... Thanks!

* If you're more an electronics person, the heart is a approximately constant-voltage generator. When resistance in the skin drops -- which is in parallel with the rest of the body "load" -- the heart has to ramp up the current in order to maintain the same voltage and thereby keep the other bits of the body running appropriately. Except the problem is even worse, because exercising muscles also become low-resistance loads, and exercise encourages the body to increase voltage (blood pressure) rather than just maintaining it.
 Perfect! I'm just a big transistor about to experience thermal runaway.
Perfect! I'm just a big transistor about to experience thermal runaway.